The closure of the Ascension Via Christi Emergency Department in Fort Scott, Kansas, would have significant implications for residents. The stand-alone ER is an essential healthcare facility that provides immediate and life-saving care to people from all walks of life, regardless of their age, socioeconomic status, or the nature of their medical concerns. It plays a crucial role in the community by addressing a wide range of healthcare needs.

Having an emergency room (ER) in Fort Scott, KS is crucial for several reasons:
- Timely Medical Care: Rural areas often have limited access to healthcare facilities, and an ER can provide timely medical care for life-threatening emergencies. The presence of an ER can mean the difference between life and death for individuals in critical condition.
- Triage and Assessment: Patients are initially triaged to determine the severity of their condition, with more critical cases receiving immediate attention.
- Treatment of Acute Injuries: Can manage acute injuries such as fractures, dislocations, sprains, strains, burns, and lacerations. They can provide stabilization and initial treatment.
- Trauma Care: Rural areas may have higher rates of accidents, including farming accidents, motor vehicle accidents, and recreational accidents. Can provide trauma care to stabilize and treat injured patients before transferring them to larger hospitals.
- Medical Emergency Care: Equipped to handle a wide range of medical emergencies, including heart attacks, strokes, respiratory distress, severe allergic reactions, and diabetic crises. Where ambulance response times may be longer, having an ER is essential to ensure that patients receive rapid and appropriate care.
- Childbirth Services: Access to obstetric care is limited and can provide vital care for pregnant women and ensure safe deliveries, reducing the risks associated with childbirth complications.
- Management of Chronic Illnesses: Can assist with the management of chronic illnesses. Can provide essential services for patients with conditions like diabetes, asthma, and heart disease.
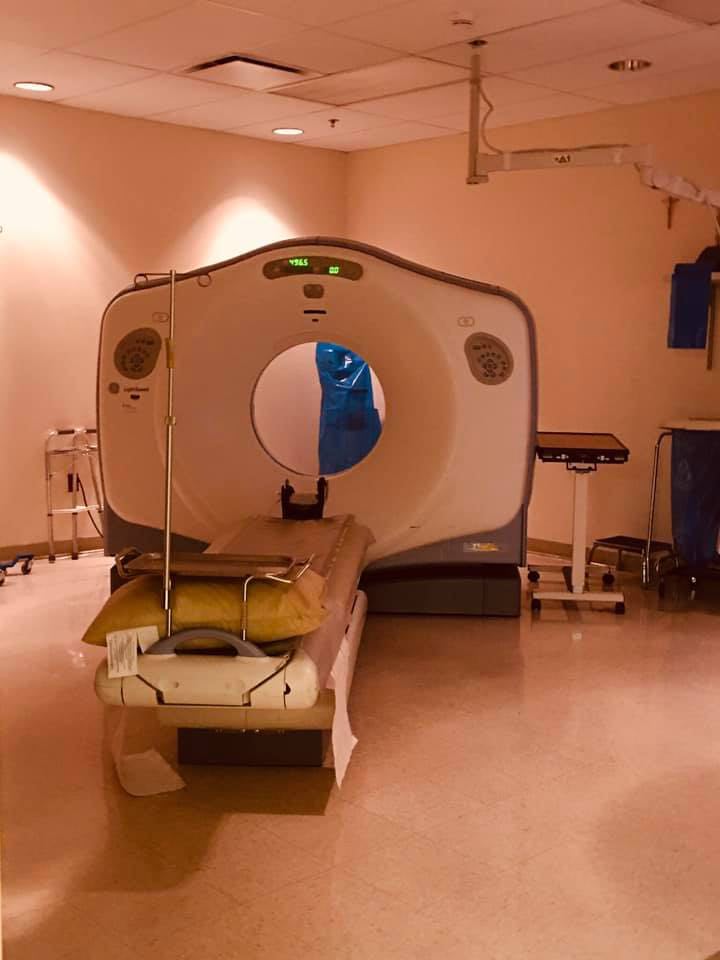
- Diagnostic Services: Have diagnostic equipment, such as X-ray machines, CT scans, and basic laboratory facilities, to assist in diagnosing patients’ conditions.
- Minor Surgical Procedures: Can perform minor surgical procedures, such as suturing wounds, draining abscesses, or setting fractures.
- Cardiac Care: Have the capability to treat cardiac emergencies, including administering medications and performing life-saving interventions like defibrillation.
- Respiratory Care: Patients with severe respiratory distress or conditions like asthma receive care, including the administration of oxygen and nebulizer treatments.
- Intravenous (IV) Therapy: Can provide IV fluids and medications for patients who require them.
- Gastrointestinal Care: Can manage conditions such as severe abdominal pain, gastrointestinal bleeding, and dehydration.
- Psychiatric Evaluation: This ER has the capability to conduct initial psychiatric assessments and provide care for individuals experiencing a mental health crisis.
- Pharmaceutical Services: Access to common medications to provide initial treatment for various medical conditions.
- Poison Control and Toxicology Services: This ER can handle cases of poisoning or exposure to toxic substances, providing treatment and coordination with poison control centers.
- Stabilization for Transfers: In cases where patients require advanced care or surgery, we can stabilize patients before arranging their transfer to a larger hospital.
- Remote and Isolated Communities: Rural areas may have remote and isolated communities where travel to the nearest city with a hospital can be time-consuming and difficult. An ER in a rural area is crucial to serve these communities and address their healthcare needs.
- Quality of Life: Having access to emergency healthcare services in rural areas improves the quality of life for residents. It provides a sense of security and encourages people to remain in these areas rather than moving to urban centers for better healthcare access.
- Preventing Overburdened Hospitals: Without ERs in rural areas, patients with non-life-threatening emergencies may flood urban hospitals, overburdening them and reducing their capacity to handle major crises. Rural ERs can help distribute the healthcare burden more evenly.
- Disaster Response: Rural areas are not immune to natural disasters, such as floods, tornadoes, wildfires, or pandemics. ERs play a vital role in disaster response by providing immediate medical assistance to those affected and coordinating disaster relief efforts.
Emergency Medical Services (EMS) and stand-alone ERs have distinct purposes, and one cannot replace the other. Here’s an overview of their roles:
Emergency Medical Services (EMS): EMS refers to the system of pre-hospital care provided by trained paramedics and emergency medical technicians (EMTs). EMS plays a critical role in the early response to emergencies, particularly in the field or at the patient’s location. EMS services typically include:
- Emergency Response: EMS personnel are dispatched to the scene of an emergency, such as car accidents, medical crises, or natural disasters.
- Assessment and Stabilization: EMS assess patients, provide immediate care, and stabilize them for transport to an appropriate medical facility. This care often involves basic life support (BLS) and advanced life support (ALS) interventions.
- Transport: EMS providers transport patients to the nearest medical facility. This may be a hospital emergency department or a stand-alone ER.
- Specialized Care: In some cases, EMS teams, especially those with paramedics, can provide more advanced care, such as administering medications, performing defibrillation, and intubating patients.
- Communication: EMS personnel maintain communication with medical control or a receiving facility to coordinate care and make informed decisions about the patient’s destination.
Stand-alone Emergency Room: We are staffed with emergency physicians, nurses, and support staff and offer a broader range of services compared to EMS. Our stand-alone ER provides:
- Comprehensive Emergency Care: We offer a full spectrum of emergency medical services, from initial triage and assessment to diagnostics and treatment of a wide range of medical conditions and injuries.
- Diagnostic Services: We have diagnostic equipment like X-rays, CT scans, and basic laboratory facilities to aid in diagnosing patients.
- Minor Surgical Procedures: Can perform minor surgical procedures, suturing wounds, and treating fractures, among other services.
- Medications and Intravenous Therapy: Have the capacity to administer medications and intravenous (IV) therapy.
- Inpatient Admissions: We are equipped to admit patients to an inpatient setting for further care when needed.
In summary, EMS and stand-alone ERs are both vital components of the emergency medical system, but they serve different roles. EMS provides pre-hospital care, rapid response, and transportation to the appropriate medical facility. Stand-alone ERs offer comprehensive emergency medical services and are staffed with healthcare professionals who can provide a higher level of care than what is typically available in the field. These two components work together to ensure that individuals in need of emergency medical care receive the most appropriate and timely assistance. They are not interchangeable but rather complementary in the overall healthcare system.
The Bourbon County EMS does an impeccable job servicing the community.
Removing our stand-alone emergency room without a suitable replacement would result in gaps in our healthcare system, potentially jeopardizing the health and safety of our residents.

The Community Health Center Of Sek Fort Scott Walk-in Clinic cannot replace the stand-alone emergency room because these two facilities serve different roles and cater to different types of medical needs.
It’s important to understand the distinctions between them:
Urgent Care Centers:
- Scope of Services: Urgent care centers are designed to provide non-life-threatening, time-sensitive medical care for conditions that require prompt attention but are not considered emergencies. They primarily handle minor injuries and common illnesses that do not pose an immediate threat to life or limb.
- Conditions Treated: Urgent care centers can address a variety of medical issues, such as minor injuries (sprains, minor fractures, cuts), common illnesses (cold, flu, ear infections), and routine healthcare services (vaccinations, physical exams, and minor preventive care).
- Convenience: Urgent care centers often have extended hours and shorter wait times compared to hospital-based ERs, making them a more convenient option for non-critical medical needs.
- No Appointments Required: Urgent care centers typically accept walk-in patients without the need for appointments.
Stand-Alone Emergency Rooms:
- Scope of Services: Stand-alone emergency rooms provide comprehensive emergency medical care and are equipped to handle a wide range of medical emergencies, including life-threatening conditions. They have the capability to perform more complex medical procedures and diagnostic tests.
- Conditions Treated: Stand-alone ERs are designed to manage severe injuries, cardiac emergencies, strokes, respiratory distress, severe allergic reactions, major trauma, and other critical medical conditions. They can provide advanced diagnostic services, such as CT scans and X-rays.
- High-Level Care: Stand-alone ERs have emergency physicians and specialized staff available around the clock, ensuring that patients receive a higher level of care for serious medical issues.
- Timely Response: Stand-alone ERs offer rapid response to life-threatening emergencies, making them crucial for situations where immediate, critical care is required.
- Patient Transfers: Stand-alone ERs can stabilize patients and facilitate their transfer to larger hospitals or specialized medical facilities when necessary.
Urgent care centers are appropriate for non-critical, non-life-threatening medical concerns. The stand-alone emergency room is essential for severe medical emergencies, trauma, life-threatening conditions, and situations requiring advanced diagnostic and treatment services.
The composition of the emergency room staff is critical for the efficient and effective functioning of the ER. Each member of the team plays a specific role in providing timely and high-quality care to patients. Here’s an overview of the importance of each role:
- Doctor or Nurse Practitioner:
- Assessment and Diagnosis: Doctors and nurse practitioners are responsible for assessing patients, making diagnoses, and determining treatment plans.
- Critical Decision-Making: They make critical medical decisions, such as ordering tests, prescribing medications, and recommending procedures.
- Treatment and Stabilization: These healthcare providers provide immediate care, stabilization, and intervention for patients with a wide range of medical conditions and emergencies.
- Coordination: They coordinate patient care, consult with specialists when needed, and ensure a smooth transfer of patients when admitted as an inpatient to a medical center.
- Nurses:
- Direct Patient Care: Nurses provide direct patient care, administer medications, monitor vital signs, and manage medical interventions as directed by the healthcare provider.
- Advocacy: They serve as patient advocates, ensuring that patients’ needs and concerns are communicated to the medical team and that their rights and preferences are respected.
- Triage: Nurses often participate in triage, prioritizing patients based on the severity of their conditions to ensure that the most critical cases receive immediate attention.
- Patient Education: Nurses provide education to patients and their families about their conditions, treatment plans, and what to expect during their ER visit.
- Emergency Room Technician:
- Assistance with Patient Care: Technicians support nurses and doctors by assisting with patient care, monitoring vital signs, and performing tasks such as wound care and specimen collection.
- Equipment and Supply Management: They ensure that essential equipment and supplies are readily available and functional for patient care.
- X-Ray and Laboratory Personnel:
- Diagnostic Services: Radiology and laboratory professionals perform diagnostic tests and imaging studies to help identify and understand the nature of a patient’s medical condition.
- Timely Results: Providing timely results from diagnostic tests is crucial for healthcare providers to make informed decisions and initiate appropriate treatment promptly.
- Front Desk Clerk:
- Patient Registration: Front desk clerks play a key role in patient registration, collecting essential information, verifying insurance, and ensuring that patients are promptly entered into the ER system.
- Communication Hub: They serve as a communication hub, relaying messages and information between patients, families, and the healthcare team.
- Hospital Flow: Front desk clerks assist in ensuring the efficient flow of patients through the ER, helping to minimize wait times and address logistical concerns.
The collective effort of this multidisciplinary team ensures that our patients receive timely, comprehensive, and compassionate care in our ER. Teamwork, communication, and coordination among these professionals are crucial to delivering the best possible outcomes for patients, especially in emergency situations where every minute can make a difference in a patient’s recovery or prognosis.
The benefits of a computed tomography (CT) scan, commonly referred to as a “CAT scan,” is a medical imaging procedure that provides detailed cross-sectional images of the body’s internal structures. CT scans are used to diagnose and evaluate various medical conditions, and they offer several valuable services, including:
- Diagnostic Imaging: CT scans are used to diagnose a wide range of medical conditions, including injuries, diseases, and abnormalities in various parts of the body. They can reveal information that may not be visible through other imaging methods.
- Visualizing Anatomy: CT scans provide clear and detailed images of bones, organs, tissues, and blood vessels. This helps healthcare professionals to understand the anatomy and structure of the body for diagnostic purposes.
- Trauma Assessment: CT scans are often used to assess traumatic injuries, such as fractures, internal bleeding, and head injuries. They can quickly identify the extent of damage and aid in treatment decisions.
- Cancer Detection: CT scans are valuable for detecting and staging various types of cancer. They can help locate tumors, assess their size, and determine if cancer has spread to other parts of the body.
- Cardiovascular Assessment: CT angiography (CTA) is a specialized type of CT scan used to visualize blood vessels and assess conditions like arterial blockages, aneurysms, and coronary artery disease.
- Pulmonary Evaluation: CT scans of the chest are used to assess lung conditions, including lung cancer, pulmonary embolism, and lung infections. They can reveal abnormalities such as nodules and masses.
- Abdominal and Pelvic Imaging: CT scans of the abdomen and pelvis are employed to investigate conditions like appendicitis, kidney stones, diverticulitis, and various gastrointestinal issues.
- Neurological Assessment: CT scans of the head can help diagnose neurological conditions, such as strokes, brain tumors, and traumatic brain injuries. They are also used to assess intracranial bleeding.
- Guiding Procedures: CT scans can be used to guide minimally invasive procedures, such as biopsies, drainage of abscesses, or the placement of catheters or needles for treatments.
- Monitoring Treatment: After a medical condition has been diagnosed and treatment initiated, CT scans can be used to monitor the progress of treatment, assess the effectiveness of interventions, and track changes in the patient’s condition over time.
- Preoperative Planning: Surgeons use CT scans to plan and prepare for surgeries by visualizing the area of interest and understanding its structure and anatomical relationships.
CT scans are a valuable tool because of their ability to provide detailed, high-resolution images quickly.
Radiology plays a crucial role in our emergency room. The importance of radiology can be summarized as follows:
- Rapid Assessment: X-rays provide a quick and non-invasive way to assess and visualize the internal structures of the body. In emergency situations, where timely diagnosis is critical, X-rays can help healthcare providers promptly evaluate injuries or conditions.
- Diagnosis of Fractures and Bone Injuries: X-rays are particularly valuable for diagnosing bone fractures, dislocations, and joint injuries. They provide clear images of bone structures, helping healthcare providers determine the type and severity of the injury, which is essential for treatment decisions.
- Detection of Foreign Objects: X-rays can identify the presence of foreign objects, such as metallic fragments or objects ingested by a patient. This information is crucial for planning appropriate interventions or surgical procedures.
- Assessment of Pneumothorax: In cases of traumatic chest injuries, X-rays are used to detect pneumothorax, a condition in which air accumulates in the pleural space around the lungs. Prompt identification is crucial for patient management.
- Diagnosis of Respiratory Conditions: Chest X-rays help in diagnosing and assessing respiratory conditions, such as pneumonia, pleural effusions, and chronic obstructive pulmonary disease (COPD).
- Evaluation of Soft Tissues: While X-rays are primarily used for visualizing bones, they can also provide information about soft tissue injuries and abnormalities, such as soft tissue swelling or the presence of gas in soft tissues.
- Diagnosis of Abdominal Conditions: Abdominal X-rays can be used to identify conditions like bowel obstructions, kidney stones, and the presence of foreign bodies in the gastrointestinal tract.
- Guidance for Procedures: X-rays are often used to guide minimally invasive procedures, such as the placement of catheters, tubes, or needles for drainage, biopsy, or pain management. This helps ensure accurate placement.
- Identification of Certain Infections: X-rays can sometimes reveal patterns associated with specific infections, such as tuberculosis, which may not be immediately evident on clinical examination.
- Monitoring Trauma Patients: In trauma cases, X-rays are essential for monitoring patients over time to assess the progression or resolution of injuries, such as fractures or pneumothorax.
X-rays are invaluable tools in our emergency room for diagnosing and assessing various medical conditions and injuries, particularly those related to bones and the chest. Their ability to provide rapid, detailed images allows healthcare providers to make timely and informed decisions, which is crucial in an emergency setting. X-rays are a key component of the diagnostic arsenal in an ER and contribute significantly to patient care and management.
In our emergency room, critical laboratory results are test findings that indicate severe medical conditions requiring immediate attention and intervention. These results are communicated to healthcare providers who promptly interpret the results quickly and initiate interventions to address the underlying medical issues and stabilize the patient’s condition. Critical laboratory results may vary depending on the specific laboratory tests conducted, here are a few examples:
- Complete Blood Count (CBC):
- Extremely low hemoglobin or hematocrit levels suggest severe anemia or acute bleeding.
- Markedly elevated white blood cell count, indicating a severe infection or leukemia.
- Chemistry Panel:
- Extremely high or low blood glucose levels may indicate diabetic ketoacidosis or hypoglycemia.
- Significantly elevated or decreased electrolyte levels, such as potassium, sodium, or calcium, can cause cardiac arrhythmias or other life-threatening complications.
- Arterial Blood Gas (ABG) Analysis:
- Severe acidosis or alkalosis in the blood indicates a critical imbalance in the body’s pH.
- Marked hypoxemia or hypercapnia, indicating significant respiratory distress.
- Coagulation Studies:
- Abnormal prothrombin time (PT) or international normalized ratio (INR), suggesting a severe coagulopathy or bleeding disorder.
- Markedly elevated activated partial thromboplastin time (aPTT), can indicate a significant risk of bleeding.
- Cardiac Enzymes and Biomarkers:
- Elevated troponin levels indicate a heart attack or myocardial infarction.
- Elevated brain natriuretic peptide (BNP) levels suggest severe heart failure.
- Blood Gas Analysis:
- Critical derangements in oxygen and carbon dioxide levels may signify acute respiratory distress or respiratory failure.
- Electrolyte and Metabolic Panels:
- Markedly high potassium levels (hyperkalemia) or low potassium levels (hypokalemia), can lead to cardiac arrhythmias.
- Severe hypernatremia or hyponatremia, can cause neurological complications and life-threatening imbalances in body fluid and electrolytes.
- Cultures and Microbiology:
- Positive blood cultures with organisms indicating severe sepsis or septic shock.
- Identification of highly antibiotic-resistant pathogens, necessitating immediate intervention.
- Hematology Studies:
- Critical low platelet count (thrombocytopenia), which can lead to severe bleeding.
- Toxicology and Drug Screens:
- Detection of life-threatening levels of drugs or toxins in the blood.
- Identification of substances that may require immediate antidote administration.
Additional laboratory testing includes several tests to evaluate various conditions. These tests include troponin, D-Dimer, BNP, myoglobin, quantitative hcg, rupture of membranes test, covid, flu, RSV, and strep. Each of these tests serves a specific purpose in diagnosing different medical conditions.
- Troponin: Troponin is a cardiac biomarker used to diagnose heart damage, specifically myocardial infarction (heart attack). Elevated troponin levels indicate cardiac muscle injury, and it’s a critical test to confirm or rule out a heart attack.
- D-Dimer: D-Dimer is a marker of blood clot formation and breakdown. It’s often used in assessing patients with suspected pulmonary embolism or deep vein thrombosis (blood clots). Elevated D-Dimer levels suggest a clotting disorder but are not specific to a particular condition. Further imaging tests are needed to confirm the diagnosis.
- BNP (Brain Natriuretic Peptide): BNP is a marker for heart failure. Elevated BNP levels can help diagnose and assess the severity of heart failure. It’s a valuable test for managing patients with cardiac issues.
- Myoglobin: Myoglobin is a protein found in the heart and skeletal muscles. Elevated myoglobin levels are often seen in conditions like rhabdomyolysis (muscle breakdown) and myocardial infarction (heart attack). It can help in the early detection of cardiac muscle injury.
- Quantitative hCG (Human Chorionic Gonadotropin): This test measures the level of the hormone hCG in the blood and is commonly used for confirming pregnancy. It can also help diagnose ectopic pregnancies and trophoblastic diseases. In non-pregnant individuals, elevated hCG levels may be indicative of certain medical conditions, such as testicular cancer or other tumors.
- Rupture of Membranes Test: This test is used to determine if a pregnant woman’s amniotic sac has ruptured (commonly referred to as “water breaking”). It’s important in obstetric care to assess the status of the amniotic fluid, which can affect the course of labor and delivery.
- COVID Testing: COVID-19 tests, including PCR and rapid antigen tests, are crucial for diagnosing active SARS-CoV-2 infections. Early diagnosis is essential to isolate infected individuals, prevent further transmission, and provide appropriate care.
- Flu Testing: Influenza (flu) tests are used to diagnose seasonal influenza infections. Distinguishing between the flu and other respiratory illnesses is important for treatment decisions and public health monitoring.
- RSV (Respiratory Syncytial Virus) Testing: RSV is a common virus that causes respiratory infections, particularly in young children and the elderly. RSV testing helps diagnose and manage RSV infections, which can be severe in certain populations.
- Strep Testing: Strep tests detect Group A Streptococcus bacteria, which can cause streptococcal pharyngitis (strep throat) and other infections. Accurate diagnosis helps guide antibiotic treatment and reduce the risk of complications.
Lactic acid testing is a valuable tool in our emergency room for several important reasons:
- Early Detection of Serious Conditions: Elevated lactic acid levels in the blood are often associated with inadequate oxygen delivery to tissues, which can be a sign of severe underlying medical conditions. It can indicate conditions like sepsis, shock, or severe hypoxia (inadequate oxygen levels), which require immediate intervention.
- Sepsis Assessment: Lactic acid levels are frequently used in assessing patients with suspected or confirmed sepsis. Sepsis is a life-threatening condition, and early detection is crucial for timely treatment to improve outcomes.
- Shock Management: In cases of various types of shock, including hypovolemic (due to severe blood loss), cardiogenic (related to heart failure), or distributive (as seen in septic shock), lactic acid levels can help assess the severity of the condition and guide treatment decisions.
- Tissue Perfusion: Lactic acid is produced when cells switch to anaerobic metabolism, usually due to inadequate oxygen supply. Monitoring lactic acid levels helps healthcare providers assess tissue perfusion (the flow of blood through tissues) and the adequacy of oxygen delivery.
- Triaging Patients: In the ER, lactic acid testing can assist in triaging patients by identifying those who require immediate attention and those who may need further evaluation or monitoring. This helps allocate resources more effectively.
- Monitoring Progress: Lactic acid levels can be tracked over time to assess the response to treatment. A decreasing level of lactic acid can indicate that interventions are improving tissue perfusion and oxygen delivery.
- Identification of Metabolic Disorders: In some cases, lactic acidosis can result from metabolic disorders, such as mitochondrial diseases. Identifying such conditions is essential for appropriate management and genetic counseling.
- Diagnostic Clarity: In cases where a patient presents with vague symptoms, lactic acid testing can provide additional diagnostic information that aids in identifying the underlying cause of illness.
- Prompt Intervention: Elevated lactic acid levels often trigger immediate medical attention, which can include administering fluids, oxygen, and other treatments to address the underlying condition, stabilize the patient, and prevent further deterioration.
- Resource Allocation: Lactic acid testing can help ER staff prioritize resources, such as admission to ICU or specialized interventions, for patients with more severe conditions indicated by elevated levels.
Lactic acid testing in our emergency room is crucial for early detection and assessment of life-threatening conditions, especially sepsis, and shock.
Blood gas analysis is a crucial diagnostic tool in our emergency room for several reasons:
- Rapid Assessment: Blood gas analysis provides immediate information about a patient’s acid-base balance and oxygenation status. This rapid assessment is vital in emergency situations where quick decisions are needed.
- Respiratory Distress: Blood gas analysis helps diagnose and monitor patients with respiratory distress or failure. It provides information about the levels of oxygen (PaO2) and carbon dioxide (PaCO2) in the blood, allowing healthcare providers to determine the severity of respiratory impairment.
- Acid-Base Balance: It assesses the patient’s acid-base status by measuring pH, bicarbonate (HCO3-), and partial pressure of carbon dioxide (PaCO2). Imbalances in these parameters can indicate conditions such as metabolic acidosis, metabolic alkalosis, respiratory acidosis, or respiratory alkalosis.
- Lactic Acid Measurement: Lactic acid levels can be assessed using blood gas analysis. Elevated lactic acid levels may indicate conditions like sepsis, shock, or tissue hypoxia, providing important information for diagnosing the underlying cause of a patient’s condition.
- Treatment Guidance: Blood gas results guide the choice and adjustment of treatments. For example, if a patient is in respiratory distress due to hypercapnia (elevated PaCO2), healthcare providers may adjust ventilation or initiate respiratory support.
- Assessing Oxygenation: Blood gas analysis provides information about the oxygen content and saturation in the blood. It helps determine whether a patient is hypoxemic (low oxygen levels), which can occur in conditions like pneumonia, pulmonary embolism, or cardiac arrest.
- Monitoring Critically Ill Patients: In the ER, critically ill patients may require continuous monitoring through arterial lines, which allow for real-time blood gas measurements. This is especially important for patients in the intensive care unit or undergoing surgery.
- Differential Diagnosis: Blood gas analysis assists in the differential diagnosis of respiratory and metabolic disorders, allowing healthcare providers to distinguish between conditions with similar symptoms.
- Treatment Evaluation: After initiating treatments, blood gas analysis helps assess the effectiveness of interventions. It allows healthcare providers to gauge whether oxygenation and acid-base balance are improving.
- Trauma Care: In cases of trauma or severe injuries, blood gas analysis can provide insights into the patient’s oxygen delivery and acid-base status, guiding resuscitation efforts.
Blood gas analysis in an emergency room is vital for rapidly assessing and diagnosing patients with respiratory distress, acid-base imbalances, and oxygenation issues. This aids in monitoring critically ill patients.
Treating altered mental status and falls in our emergency room is important for several reasons:
Altered Mental Status:
- Diagnostic Challenge: Altered mental status can result from various underlying causes, including neurological conditions, intoxication, metabolic imbalances, infections, and more. Prompt evaluation and diagnosis in the ER are critical to identify the root cause and initiate appropriate treatment.
- Potential Life-Threatening Conditions: Altered mental status can be a sign of severe medical conditions, such as stroke, seizures, diabetic emergencies, or head injuries. Treating these conditions in a timely manner can prevent further deterioration and reduce the risk of complications.
- Safety Concerns: Patients with altered mental status may be disoriented, agitated, or unresponsive. Ensuring their safety and preventing self-harm or harm to others is a top priority in the ER.
- Reversible Conditions: Some causes of altered mental status, such as medication side effects or certain infections, are reversible with prompt medical intervention. Treating these causes can lead to a complete recovery.
- Decision-Making Capacity: Patients with altered mental status may lack the capacity to make informed medical decisions. Medical professionals in the ER must assess and provide appropriate care, which may include decisions related to medical treatment, consent, or guardianship.
Falls:
- Injury Prevention: Falls are a leading cause of injuries, especially among older adults. Treating patients who have fallen in the ER can help identify and address injuries such as fractures, head trauma, and internal bleeding, reducing the risk of complications.
- Fracture Detection: Falls can result in fractures, particularly hip fractures, which can be painful and limit mobility. Early diagnosis and treatment can improve the chances of a successful recovery.
- Head Injury Assessment: Falls that lead to head injuries, even seemingly minor ones, require thorough evaluation. This is essential for detecting traumatic brain injuries and ensuring proper care to prevent long-term consequences.
- Underlying Medical Conditions: Falls may be symptomatic of underlying medical conditions, such as dizziness, syncope (fainting), or balance issues. Identifying and addressing these conditions can prevent future falls.
- Preventing Recurrence: Identifying the circumstances and risk factors that led to a fall allows healthcare professionals to develop strategies and interventions to reduce the risk of future falls.
- Psychosocial Support: Falls can have a significant psychosocial impact on individuals, leading to anxiety, fear of falling again, or decreased quality of life. Providing support and resources to address these aspects is essential in the ER.
- Rehabilitation and Follow-Up: Patients who have fallen may require rehabilitation or additional medical follow-up. The ER can initiate this process, ensuring that patients receive the necessary care and support after their visit.
Treating altered mental status and falls in the emergency room is vital to addressing acute medical issues, preventing complications, and providing appropriate care and support. It ensures the safety and well-being of patients, particularly those who are vulnerable due to their condition or age, and it plays a critical role in preventing further harm and promoting recovery.
Patients are often referred to our emergency room from various healthcare facilities, including Community Health Centers (CHC) and Medicalodges. These referrals occur when individuals require immediate medical attention or treatment beyond what can be provided at the referring facility.
Our emergency room’s care encompasses a wide variety of medical conditions and situations, including chest pain, atrial fibrillation (A-fib), arrhythmias, respiratory distress, weakness, nausea, vomiting, diarrhea, fluctuations in blood pressure, pneumonia, edema, defibrillator alerts at home, allergic reactions to brown recluse spider bites, abdominal pain, seizures, intracranial bleeding, cough, fever, septic urinary tract infections (UTIs) and various infections, rectal bleeding, wounds, speech difficulties, tumors, patients at risk of self-harm or harm to others, motor vehicle accidents, expectant mothers, code blue emergencies, police-ordered blood draws, and medical assessments for incarceration clearances, among others.
Our ER’s capacity to handle a diverse range of cases is extensive, and the examples provided here represent only a fraction of the medical issues and scenarios that we address.
Our ability to admit patients to an inpatient hospital setting or higher level of care is crucial for several reasons:
- Continuity of Care: In some cases, patients who initially present to the ER may have complex or serious medical conditions that require ongoing treatment and monitoring. Admitting them to a hospital allows for continuous care, including observation, further diagnostic tests, and specialist consultations if necessary.
- Timely Treatment: Admitting a patient ensures they receive timely and appropriate treatment and interventions. It allows healthcare providers to address the underlying medical condition more effectively and promptly, which is especially important in critical or severe cases.
- Specialized Care: Admitting a patient to a hospital provides access to a broader range of medical specialists, advanced diagnostic equipment, and medical interventions.
- Severe or Progressive Conditions: For patients with medical conditions that may deteriorate or progress rapidly, admission to a hospital allows for close monitoring and immediate response to any changes in their condition. This is crucial in cases like heart attacks, strokes, or severe infections.
- Surgical Intervention: When a patient requires surgery, the hospital is equipped with operating rooms and surgical teams. Patients admitted from the ER can be prepared for surgery as needed, minimizing delays in critical surgical interventions.
- Inpatient Care: Hospitalization can provide a more controlled and secure environment for patients who require inpatient care, including those with serious infections, chronic medical conditions, or mental health issues.
- Access to Specialized Units: Hospitals have specialized units, such as intensive care units (ICUs), neonatal ICUs, and burn units, which may be necessary for certain patients admitted from the ER.
- Diagnostics and Testing: Hospitals typically have a broader range of diagnostic tests and imaging services, allowing for a more comprehensive evaluation and monitoring of patients.
- Support Services: Hospitals can offer additional support services, such as physical therapy, occupational therapy, and social services, which may be essential for the recovery and rehabilitation of some patients.
- Infection Control: For patients with contagious diseases, hospitals have isolation and infection control measures in place to prevent the spread of infections to healthcare providers and other patients.
- Access to Specialists: Hospitals have access to a wide array of specialists, including cardiologists, neurologists, orthopedic surgeons, and many others, ensuring that patients receive the right expertise for their specific conditions.
We ensure that individuals with complex, severe, or rapidly progressing medical conditions receive the necessary care, treatment, and monitoring in an environment that offers the resources and expertise needed for their recovery and well-being. It allows for a seamless transition between emergency care and inpatient care, contributing to better patient outcomes.
The presence of the helipad at our emergency room facility with the capability to airlift or “life-flight” patients via helicopter is of significant importance for several reasons:
- Rapid Response to Critical Cases: Helipads enable the rapid transport of critically ill or injured patients to the ER. This is especially crucial for cases like trauma, heart attacks, strokes, or severe medical emergencies where time is a critical factor in patient outcomes.
- Extended Reach: A helipad expands the geographical reach of the ER, allowing it to serve patients from a wider area, including remote or rural regions where ground transportation may be time-consuming or impractical.
- Specialized Care: In some situations, patients require specialized care that may not be available at local hospitals. Helicopter transport ensures these patients can reach a facility with the necessary resources and expertise.
- Time-Critical Interventions: Certain medical interventions, such as surgeries or administration of specific medications, must be performed within a narrow time window. Helicopter transport can significantly reduce the time it takes to get patients to the ER for these interventions.
- Disaster Response: In the event of natural disasters, mass-casualty incidents, or other emergencies, helipads enable a quick response to evacuate and treat multiple patients, helping to alleviate the strain on local healthcare resources.
- Pediatric and Neonatal Transport: Helicopter transport is crucial for transferring pediatric and neonatal patients to facilities with specialized pediatric care units.
- Remote and Inaccessible Areas: In regions with limited road access, such as mountainous terrain or islands, helipads are essential for providing healthcare access.
- Weather and Traffic Considerations: Helicopters are less affected by adverse weather conditions and traffic congestion, allowing for more reliable and timely patient transport, especially in emergencies.
- Resource Sharing: Helipads facilitate the sharing of medical resources, as medical teams and equipment can be rapidly transported to or from the ER to assist in patient care.
- Survival and Outcomes: Swift access to the ER through helicopter transport can improve patient survival rates and outcomes, particularly for those with time-sensitive conditions.
- Community Preparedness: Having a helipad reflects the ER’s commitment to community health and preparedness, providing reassurance to residents that the facility is well-equipped to handle emergencies.
A helipad at the ER provides a crucial lifeline for patients needing urgent and specialized care, regardless of their location. It plays a vital role in saving lives and improving patient outcomes, making it an indispensable feature for emergency medical services.

Our emergency room plays a crucial role in addressing the needs of mental health patients, especially during mental health crises or when individuals are experiencing acute psychiatric symptoms. Here’s an overview of the need for mental health services in our emergency room, including assessment and potential admission:
Need for Mental Health Services in the Emergency Room:
- Crisis Intervention: The ER is often the first point of contact for individuals experiencing acute mental health crises. We provide a place for immediate assessment and intervention when a person’s well-being is at risk.
- Safety and Stabilization: We are equipped to provide a safe and secure environment for individuals in crisis, ensuring that they are protected from harm to themselves or others. This is essential for stabilizing their condition.
- Accessibility: We are available 24/7, making us accessible to individuals in need of urgent mental health care, regardless of the time of day or night.
- Assessment: We have the necessary resources and personnel to conduct mental health assessments, including evaluating the severity of a person’s condition, assessing the risk of harm, and determining appropriate next steps.
Mental Health Assessment in the Emergency Room:
- Triage: Individuals seeking mental health care in the ER are triaged to assess the urgency of their situation. Those at immediate risk of self-harm or harm to others are given priority.
- Initial Evaluation: A mental health professional conducts an initial evaluation to gather information about the individual’s mental health history, symptoms, and current crisis. Medical staff may also perform a physical examination to rule out underlying medical causes of psychiatric symptoms.
- Risk Assessment: An assessment of the individual’s risk level is essential to determine the appropriate level of care. This includes assessing the risk of suicide, self-harm, harm to others, or inability to care for oneself.
- Stabilization: The primary goal is to stabilize the individual’s condition. This may involve medication, counseling, or other interventions to alleviate acute symptoms and ensure safety.
- Treatment Plan: Following assessment and stabilization, a treatment plan is developed. This may involve outpatient care, referral to psychiatric services, admission to an inpatient psychiatric unit, or other appropriate services.
Admission to Inpatient Psychiatric Care:
- Medical Necessity: Admission to an inpatient psychiatric unit is considered when an individual’s mental health condition is severe, and there is a substantial risk to their safety or the safety of others. Medical necessity and the need for intensive psychiatric care are primary factors in determining admission.
- Legal Criteria: Admission to a psychiatric facility may be based on legal criteria, such as involuntary commitment or court-ordered treatment when an individual is deemed to pose a significant risk.
- Assessment by Psychiatrist: A psychiatrist plays a key role in evaluating the need for inpatient care. They assess the individual’s symptoms, risk factors, and response to initial treatment.
- Length of Stay: The length of inpatient psychiatric stays varies depending on the individual’s condition. The goal is to stabilize the person, develop a longer-term treatment plan, and ensure they are safe to return to the community.
- Multidisciplinary Care: Inpatient psychiatric units provide comprehensive care, including medication management, therapy, group therapy, and support to address the individual’s mental health needs.
The need for mental health services in our ER, along with proper assessment and admission when necessary, is essential for providing timely and appropriate care to individuals in mental health crises. It helps ensure their safety, stabilization, and access to the right level of mental health support.
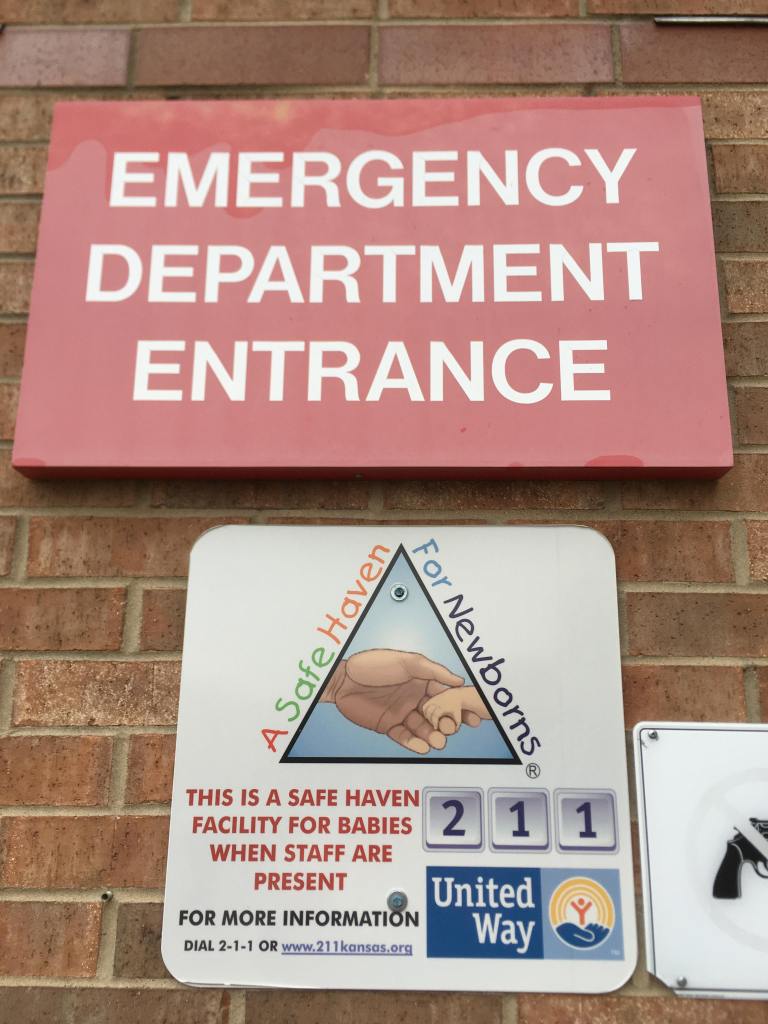
This emergency room provides a “Safe Haven” drop, often referred to as a “Baby Drop-Off,” which is a secure location where a parent or guardian can safely and anonymously surrender an unwanted infant. A safe haven for newborns can mean life or death for that infant in the time of a mother’s crisis.
Medical jail clearances, often referred to as medical clearance or medical assessments, are essential for law enforcement when dealing with individuals who require medical attention while in police custody, especially those who have been arrested, detained, or brought to our emergency room for various reasons. The importance of medical jail clearances from the ER for police includes the following:
- Patient Safety and Well-being: The primary concern during a medical jail clearance is the health and safety of the individual in police custody. Medical assessments conducted in the ER ensure that any existing medical conditions, injuries, or illnesses are promptly identified and addressed.
- Identification of Medical Conditions: Medical jail clearances help identify medical conditions that may not have been apparent during the arrest or initial processing. This information is crucial for providing appropriate medical care and ensuring that the individual’s rights and well-being are protected.
- Treatment of Injuries and Illnesses: If the person in custody requires medical treatment for injuries or illnesses, the ER is equipped to provide immediate care. Law enforcement relies on the medical staff in the ER to treat the individual appropriately, ensuring that they receive the necessary care.
- Determining Fitness for Detention: In some cases, individuals may be too ill or injured to be safely detained in a jail or detention facility. Medical jail clearances help determine whether a person is medically fit for detention. If not, alternative arrangements, such as hospitalization, may be required.
- Documentation: Medical assessments in the ER help document the individual’s medical condition, which can be valuable for legal and administrative purposes. This documentation can serve as evidence in legal proceedings, establish a baseline for the individual’s health, and record any injuries or illnesses.
- Legal Compliance: Conducting medical jail clearances in the ER is a crucial aspect of ensuring that law enforcement complies with legal and ethical standards. It demonstrates a commitment to the health and well-being of individuals in custody and can help prevent claims of neglect or mistreatment.
- Minimizing Liability: By seeking medical clearance and treatment when necessary, law enforcement can minimize potential liability and legal consequences associated with neglecting the medical needs of individuals in custody.
- Chain of Custody: For individuals who need to be returned to custody after receiving medical care, medical jail clearances establish a clear chain of custody, ensuring that individuals are properly accounted for and documented.
- Professional Collaboration: Collaboration between law enforcement and healthcare professionals in the ER fosters a sense of professionalism and respect for individual rights, contributing to the overall quality of law enforcement and healthcare services.
- Humanitarian Considerations: Providing individuals in custody with access to appropriate medical care in the ER reflects a humanitarian approach to law enforcement, emphasizing care, dignity, and the preservation of life.
In summary, medical jail clearances from our emergency room are essential for protecting the health and well-being of individuals in police custody, ensuring they receive proper medical care, and complying with legal and ethical standards. This practice helps safeguard the rights of those in custody and contributes to a more humane and professional approach to law enforcement.
The need for law enforcement to bring a suspect to the hospital for a blood draw arises in certain situations, primarily for legal, investigative, and public safety reasons. Here are some common scenarios in which law enforcement may require a suspect to undergo a blood draw at our hospital:
- DUI Investigations: In cases of suspected driving under the influence (DUI) or driving while impaired (DWI), law enforcement may bring a suspect to our hospital for a blood draw to determine their blood alcohol content (BAC) or the presence of drugs. Blood tests can provide more accurate and reliable evidence of impairment compared to breathalyzer tests.
- Search Warrants: When police have obtained a search warrant that specifically authorizes a blood draw, they may take a suspect to our hospital to ensure compliance with the warrant. This typically occurs in cases where there is probable cause to believe that the suspect’s blood contains crucial evidence related to a crime.
- Accidents and Injuries: If a suspect is involved in an accident or incident resulting in injuries, law enforcement may take them to our hospital for a blood draw to determine their medical condition and screen for substances that could have contributed to the incident.
- Medical Emergency: In cases where a suspect is experiencing a medical emergency, law enforcement may bring them to our hospital for both medical treatment and, if necessary, a blood draw. This is done to ensure the person’s immediate health needs are addressed and to obtain evidence for potential legal proceedings.
- Search for Controlled Substances: If law enforcement has reason to believe that a suspect has ingested or concealed controlled substances, they may seek a blood draw to recover evidence for drug-related offenses.
- Non-Consensual Blood Draws: In situations where a suspect refuses to provide a voluntary blood sample and law enforcement has legal grounds to obtain a sample, they may bring the suspect to our hospital for a non-consensual blood draw, typically with a warrant or based on specific legal justifications.
- Evidentiary Purposes: Blood draws are often used to gather evidence in cases where other forms of evidence, such as breath tests, urine tests, or field sobriety tests, are inconclusive or unavailable.
- Investigative Leads: Blood draws can yield critical information in criminal investigations, such as identifying intoxicants, substances, or medical conditions relevant to a crime.
It’s important to note that blood draws for law enforcement purposes must adhere to legal and constitutional standards, including obtaining proper consent, search warrants, or legal justifications, depending on the specific circumstances and jurisdiction. Suspects have rights and protections under the law, and the procedures followed must comply with these rights.
The chain of custody is a legal procedure that documents the chronological history of a piece of evidence, ensuring its integrity, security, and authenticity throughout its handling. While it is often associated with drug urine tests, the need for law enforcement’s involvement in maintaining the chain of custody for such tests in our emergency room may vary depending on the specific circumstances and legal requirements. Here are situations where police involvement in the chain of custody for drug urine tests in the ER may be necessary:
- Criminal Investigations: When a patient’s urine sample is collected as part of a criminal investigation, especially in cases involving drug-related offenses, law enforcement is typically responsible for establishing and maintaining the chain of custody to preserve the evidentiary value of the sample.
- Legal Proceedings: If a urine test result is expected to be used as evidence in legal proceedings, such as court cases or criminal trials, the involvement of law enforcement in establishing and maintaining the chain of custody is crucial to ensure that the test results are admissible in court.
- Court-Ordered Testing: In cases where a court has issued an order for urine testing, law enforcement may be responsible for handling the collection process and maintaining the chain of custody to comply with the court’s directive.
- Public Safety Concerns: In situations where a patient’s drug use is suspected to pose an imminent threat to public safety, law enforcement may become involved in the urine testing process to ensure the proper identification and legal handling of the evidence.
The specific need for police involvement in maintaining the chain of custody for drug urine tests in our ER will depend on the circumstances and the legal and investigative requirements of each case. The goal is to ensure the integrity of the evidence for any potential legal or investigative proceedings while upholding patient rights and privacy.
Admission to hospice care from our emergency room is a process that can occur under specific circumstances when a patient’s condition is determined to be terminal or incurable, and the focus of care needs to shift from curative to palliative care. Here is an overview of how admission to hospice care from the ER typically occurs:
- Medical Evaluation: When a patient with a serious illness or life-limiting condition presents to the ER, the medical team conducts a thorough evaluation to assess the patient’s current condition and prognosis. This evaluation may include reviewing the patient’s medical history, conducting diagnostic tests, and consulting with specialists.
- Shared Decision-Making: If it is determined that the patient’s condition is terminal and curative treatments are no longer effective or desired by the patient, the medical team will engage in shared decision-making with the patient and their family or designated decision-makers. This process involves discussing the prognosis, treatment options, and the goals of care.
- Referral to Hospice: If the patient, family, or designated decision-makers express a preference for comfort-focused care at the end of life, the medical team may initiate a referral to a hospice care provider. Hospice care focuses on managing pain and symptoms, providing emotional and spiritual support, and enhancing the patient’s quality of life.
- Transition to Hospice Care: If the patient and their family choose to proceed with hospice care, arrangements will be made for the patient’s transition to a hospice facility or their home, depending on their preference and circumstances.
- Coordination of Care: The ER medical team will collaborate with the hospice team to ensure a smooth transition of care. The patient’s medical records and care plan will be shared with the hospice provider to ensure continuity of care.
- Palliative Care Management: Hospice care focuses on managing pain, alleviating symptoms, and providing emotional and spiritual support. A team of healthcare professionals, including nurses, physicians, social workers, and chaplains, may be involved in the patient’s care.
- Emotional and Spiritual Support: Hospice care also offers support to the patient’s family, helping them navigate the emotional and practical aspects of end-of-life care.
- Regular Reassessments: Hospice providers regularly reassess the patient’s condition and make adjustments to the care plan as needed to ensure comfort and quality of life.
Admission to hospice care is a patient-centered decision that involves careful consideration of the patient’s wishes, medical condition, and overall goals of care. It aims to provide comfort, dignity, and support to individuals and their families during the final stages of life. Hospice care focuses on maintaining the patient’s comfort and quality of life, rather than pursuing curative treatments, and can be provided in various settings, including the patient’s home or a hospice facility.
When a patient passes away in the emergency room, the hospital staff will typically follow a set of procedures:
- Notification: Hospital staff will notify the patient’s family or next of kin about the patient’s passing. They will provide support and guidance during this difficult time.
- Documentation: The hospital will complete the necessary documentation related to the patient’s death, including a death certificate.
- Transfer to the Morgue: If the family does not have a specific funeral home in mind, the hospital may assist by transferring the deceased patient to the hospital morgue.
- Release to Funeral Home: The family, in consultation with the hospital staff, will typically choose a funeral home to handle the deceased person’s final arrangements. The chosen funeral home will then arrange for the transfer of the deceased from the hospital morgue.
- Funeral Arrangements: The funeral home will assist the family in making funeral or memorial service arrangements, cremation, or burial, as per the family’s wishes.
Funeral homes and morgues typically operate independently and handle these services according to the family’s preferences and legal requirements.
The absence of our local emergency room and the need for patients to travel significant distances (27 to 35 miles) for emergency care can indeed place a considerable burden on individuals in need of urgent medical attention. This situation can have several negative consequences and challenges for both patients and the community:
- Delayed Access to Care: The most immediate and significant concern is the delay in receiving emergency medical care. In critical situations, such as heart attacks, strokes, severe injuries, or life-threatening illnesses, every minute counts. Delayed access to care can lead to poorer patient outcomes and a higher risk of complications or mortality.
- Transportation Challenges: Traveling such distances to reach an emergency room can be difficult, especially in rural areas with limited public transportation options. Patients may struggle to arrange transportation, which can further delay their arrival at the hospital.
- Increased Stress and Anxiety: Patients and their families may experience heightened stress and anxiety when facing a medical emergency, made worse by the additional stress of a long journey to receive care.
- Potential for Deterioration: The longer the delay in accessing care, the greater the risk of a patient’s condition worsening. For example, a minor injury that could be easily treated in a timely manner might become more severe and complicated over an extended journey to a distant ER.
- Impact on Community Health: The absence of local emergency care can negatively impact the overall health and safety of the community. People may hesitate to seek care due to the distance, and this can lead to missed opportunities for early intervention and prevention.
Statistics and studies have shown a clear correlation between delayed emergency care and poor patient outcomes. Timely intervention in emergency medical situations often makes the difference between recovery and complications, disability, or death.
The availability of local emergency care is a critical component of public health, and its absence or inadequacy can have profound consequences for patient well-being and community health.
An urgent care facility may refuse to provide medical services to individuals who do not have insurance coverage. On the other hand, emergency rooms are obligated to treat everyone, regardless of their ability to pay.
The Ascension Via Christi Emergency Department in Fort Scott, Kansas is reportedly closing by the end of the year. CHC/SEK is not interested in providing emergency room services to Fort Scott. The building is owned by Legacy Health. In an effort to ensure ongoing emergency services in Fort Scott, Legacy Health is collaborating with Bourbon County and Amberwell Health.
Amberwell is known for its unwavering commitment to strengthening healthcare in rural communities. With a mission deeply rooted in serving these underserved regions, Amberwell has been making a significant impact by bridging the gap in healthcare access.
Recognizing the unique challenges faced by rural communities, Amberwell strives to provide comprehensive and accessible healthcare services to individuals residing in these areas. By establishing clinics, hospitals, and healthcare facilities in rural communities, Amberwell aims to bring quality medical care closer to the people who need it the most. Amberwell also actively collaborates with local organizations, government agencies, and healthcare professionals to create a comprehensive network of support.
In conclusion, Amberwell’s mission to strengthen healthcare in rural communities is driven by its unwavering dedication. Through their tireless efforts, Amberwell is making a profound difference in the lives of individuals living in rural areas, ensuring that they have access to the healthcare they deserve.